
During pregnancy, a woman's body undergoes dramatic changes. The hormonal background changes completely, adapting to pregnancy and childbirth. As a result, the tone of the vein wall decreases, its permeability increases, and microcirculation deteriorates. Varicose veins during pregnancy often spread to the lower part. Treatment of varicose veins during pregnancy should be timely and correct so as not to harm the child.
Cause
Varicose veins are common during pregnancy. The more time a woman spends in one position, the greater the likelihood of such a pathology. The body is also heavily influenced by genetic predisposition. The period of childbirth, especially the second and third trimester, is the main provocative factor in the development of varicose veins in women.
This pathology is caused by the fact that the blood vessels in the lower part of the legs and pelvis experience excessive and prolonged pressure. For a long time, blood vessels perform their functions to the maximum. The ever-growing uterus puts a lot of pressure on the vein walls. This creates an obstacle to the full microcirculation of blood in the lower part of the foot.
Also, another reason for varicose veins during pregnancy is constant weight gain. On average, a woman gains about ten kilograms over the course of nine months. And this is an additional burden on the ship. As a result, the veins in the lower part of the leg swell and greatly expand, causing a severe stretch along the entire length. If there is a genetic predisposition to varicose veins, it is important to take preventive measures in time. Traditional medicine, which suggests using unconventional methods - baths, compresses, is effective in preventing varicose veins during pregnancy.
Women whose work involves standing or sitting for long periods have to deal with varicose veins during pregnancy more often. Also susceptible to this disease are women who abuse long periods of walking in high-heeled shoes. It is recommended to avoid wearing such products every day and limit yourself to options with a heel height of no more than three centimeters.
Development factors
Factors that provoke the development of varicose veins of the legs during pregnancy are:
- Not being physically active or leading a sedentary lifestyle.During pregnancy, especially in the last trimester, physical activity cannot be avoided. Sometimes complete restriction of movement is the key to preserving the fetus; the woman had to stay in bed most of the time. As a result, the veins of the lower legs suffer, the tone of the blood walls decreases, and the access of blood and oxygen to the legs worsens. The result is the development of varicose veins.
- Increased load on the venous network.During pregnancy, a woman always gains weight. Blood pressure increases, and compression occurs in the veins. The expansion of the wall becomes continuous, and this is fraught with irreversible pathological processes.
- Dramatic changes in hormone levels.During pregnancy, a rapid increase in progesterone levels occurs. This hormone is responsible for the normal course of pregnancy and the maintenance of the fetus. But it has a negative effect on the vascular system, causing the blood walls to stretch, and they begin to overflow with blood.
This disease can cause disorders in the hematopoietic system. With increased blood clotting, circulation slows down. Stagnation occurs in the veins, the walls begin to expand under blood pressure. Other causes of the disease include:

- rapid weight gain - this happens if a woman does not eat properly;
- the network of capillaries and spider veins that were present before the child was conceived;
- repeated pregnancy;
- waxing;
- carry heavy objects;
- prolonged exposure to direct sunlight.
Gynecologists and phlebologists are not tired of talking about whether varicose veins affect pregnancy. Because with impaired blood circulation and poor oxygen access to internal organs, not only women, but also children suffer.
symptoms
The first symptom of the development of such a pathology is visual changes. In the early stages, nets and stars appear on the surface of the epidermis. Veins become clearly visible. Their color becomes bluish, yellowish or greenish. If mild varicose disease develops, the pathology does not develop outside the vascular network.
But if the disease reaches a severe level, the epidermis changes - pain appears during varicose veins during pregnancy, thickening, and redness. In this case, we can talk about the early form of thrombophlebitis, which develops during pregnancy. Comes with the following clinical pictures:
- severe swelling of the lower part;
- constant itching and burning in the affected area;
- increased dryness of the epidermis;
- pain, convulsions, especially at night;
- heaviness after physical activity, a long walk, or even after a small walk;
- Ulcers appear on the epidermis, which are difficult to get rid of.
The pain in the leg is reduced if you lift it. Some women only face external defects in the form of spider veins, while others experience unpleasant symptoms, the intensity of which gradually worsens. If treatment is not carried out, various complications arise in the form of blood clots, phlebitis and trophic ulcers.
Signs
During pregnancy, you need to monitor your health, monitor any changes and consult a doctor in time. Symptoms of varicose veins during pregnancy:
- legs, ankles and feet become swollen, swollen and painful;
- attacks of spasms and spasms appear in the hips and legs, especially at night;
- heaviness in the lower part of the legs, especially in the afternoon;
- itching, burning, increased dry skin;
- clearly visible veins on the surface of the skin;
- ulcers on the epidermis, which are difficult to treat and do not heal for a long time;
- painful sensation, the intensity of which decreases if you raise your leg.
Varicose veins can spread not only to the lower legs. There are other organs that experience high pressure during pregnancy. Varicose veins of the external genitalia and vagina often develop. Varicose veins can be visually seen on the perineum, partially affecting the buttock area. The clinical picture for this disease looks like this:
- interesting discomfort and pain, the nature of pain appears in the lower abdomen;
- during defecation there is a disturbing pain;
- burning sensation felt when emptying the bladder;
- after emptying the bladder, itching and tingling are felt;
- During intimacy, unpleasant sensations arise.
It is impossible to make a diagnosis based on external examination alone. In addition, you need to undergo diagnostic steps.
Varicose veins by trimester
First trimester

In the first trimester of pregnancy, varicose veins often occur in latent form. External signs of varicose veins in the early stages of pregnancy are limited to barely noticeable spider veins, tired legs, and discomfort after long walks. At this stage, you should not ignore such symptoms, it is better to contact a phlebologist first to avoid further development of the pathological process. Properly selected venotonics, baths and lotions will help stop the progression of the disease.
Second trimester
Varicose veins during pregnancy in the 2nd trimester are more noticeable. The constant pressure from the growing uterus and the heavy load on the legs have a negative effect on blood circulation and affect oxygen access.
Third trimester

In the 3rd trimester of pregnancy, varicose veins manifest themselves intensively in the absence of preventive measures in the early stages. Severe swelling of the legs, itching and tingling of the skin, and attacks of night cramps appear. Correctly selected therapy will help to overcome such manifestations.
Diagnostics
If the superficial veins are affected, the doctor may suspect the development of varicose veins after the first examination. During the consultation, the phlebologist collects anamnesis data and takes into account the patient's complaints. To make a correct diagnosis, the following types of examinations are prescribed:
- general urine analysis;
- clinical blood tests;
- study of biochemical blood parameters;
- ultrasonography;
- duplex scanning;
- If necessary, magnetic resonance imaging may be prescribed.
Treatment
During pregnancy, conservative therapy methods are used to treat varicose veins:
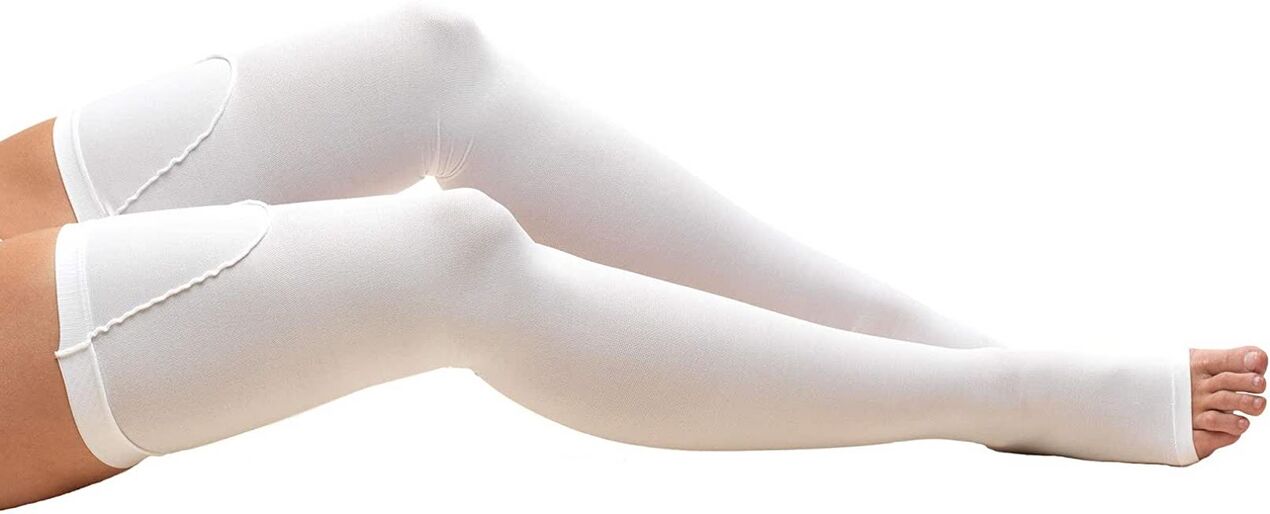
- Wear medical knitwear that has compression properties.Shapewear, stockings, tights and knee socks are encouraged. Thanks to this knitwear, the vessels are kept in the right condition, the veins do not expand, and the blood flow improves. Wearing such a product is indicated throughout the day, and if there are problems with veins, stockings are also not removed at night.
- Use properly fitted shoes.Products with stilettos, platforms and high heels are prohibited. When regularly wearing such shoes, there is a high load on the muscles of the lower leg, natural blood circulation deteriorates, and fatigue quickly appears. It is recommended to choose comfortable and stable shoes with low heels.
- Dosed physical activity.During varicose veins during pregnancy, congestion occurs, so you need to get rid of them. To do this, it is recommended to swim, walk more, and do special therapeutic exercises.
- Maintain a proper diet.To make the walls of blood vessels stronger, it is recommended to include in the menu foods rich in ascorbic acid, tocopherol, nicotinic acid, and B vitamins. Products containing potassium, magnesium, and manganese will also be useful. The diet should contain foods high in fiber. They are a good prevention against constipation.
If the doctor considers it appropriate, local drugs may be prescribed - gels, ointments, creams, which are venotonics and phlebotonics in their action. During pregnancy, the choice of medicine must be correct so as not to cause complications. Ointments containing glycosaminoglycan are effective and safe. They prevent blood clotting and the formation of blood clots. Venotonic can be used from the 2nd trimester. They have anti-edematous, anti-inflammatory and vascular strengthening properties.
In advanced cases, the disease is treated with surgery. Such methods are used only when there is a threat of thrombophlebitis. The modern treatment method is sclerotherapy.

What else does a phlebologist recommend to alleviate the condition:
- often raise your legs;
- after a day's work, soak your feet in warm water with dissolved sea salt for half an hour;
- do not cross your legs, do not throw them over each other, so as not to interfere with blood circulation;
- change body position frequently, warm up periodically;
- sleep on your left side;
- control the consumption of salty foods;
- control weight.
Prevention
Preventive measures will reduce the load on the legs and increase blood flow. It is recommended to take a comfortable position for the body more often, and raise your legs to a high position as often as possible. This ensures the outflow of blood and lymph fluid and prevents stagnation.
During the day, periodically do simple gymnastics - stretch your toes and heels, make circular movements with your toes. To ensure proper blood microcirculation, it is important to eat right, swim, and walk more.
It is important to avoid wearing tight and uncomfortable products, platform shoes and heels. Tight pants and tight socks are prohibited. It is recommended to arrange different foot baths. Refrain from visiting bathhouses and saunas, and don't take hot showers.
Following simple rules will help prevent the appearance of pathological processes in blood vessels. If the early signs of varicose veins appear, you should visit a phlebologist as soon as possible. After the examination, the doctor will decide how to proceed. It is forbidden to use any medicine on your own.


















